Patient Stories
Cancer Care
Beating Breast Cancer: Michelle Miller
Survivor Michelle Miller relies on friends, family and a committed care team.
Michelle Miller knew when she felt the lump in her breast that there was no time to waste.
"I saw my primary care doctor within two days," she said. "Then came mammograms and biopsies, and two weeks after I found the lump, I was in surgery. It was stage III breast cancer, so my team at Lake Regional Cancer Center took a very aggressive approach."
Reason to Fight
Miller was 41 at the time of her breast cancer diagnosis. She worked at Petco in Osage Beach as a dog trainer and spent much of her free time volunteering with rescued dogs. She and her husband, Mike Martin, who live in Kaiser, also have four dogs of their own.
Miller understood her diagnosis was serious but not hopeless. According to the American Cancer Society, the five-year survival rate for stage III breast cancer is about 72 percent.
"Hearing the 'c' word was definitely scary," Miller says. "But, I tried to keep my spirits up because I know the attitude of the patient is important. I also had lots of support through family and friends, and my work was wonderful to me."
Close-to-Home Care
Originally from Columbia, MO., Miller first thought she would go there for treatment. When she realized how difficult traveling back and forth would be, she decided to give Lake Regional a look.
"It was very convenient to come here, and everybody here was very attentive and compassionate," she says. "If there was anything I needed, there was someone here I could turn to for help."
Along with going to Lake Regional Cancer Center for her radiation and chemo, Miller also went to Lake Regional General Surgeon John Patton, D.O., FACOS, for surgery to remove the tumor and 13 lymph nodes. Nine of the 13 had cancer.
"20 years ago, I wouldn't have made it," Miller says. "Lake Regional saved my life."
Finding HOPE
Miller also drew support from Lake Regional's HOPE Program. This program is funded by community donations and provides various forms of help to local cancer patients. Unable to work during her eight months of treatment, Miller was grateful to receive gas cards and other financial assistance.
"I also went to the Look Good…Feel Better," Miller says, referring to a class that helps women with makeup tips, skin and nail care, and coping with hair loss. "And I went to Hope for Women, a support group for women with cancer. It was a good confidence-builder, and it helped me to be around other women in my same situation."
Never Alone
After surgery, four months of chemo and six weeks of radiation, Miller moved on to tamoxifen, a pill she will take for at least 10 years. It has been two years since her final radiation treatment, and Miller is feeling great.
"When I was first diagnosed, one of my friends said she didn't have to worry about me because I'm too ornery to let cancer get me," says Miller, smiling. "Beating cancer is not an easy thing to do, and I certainly didn't do it alone."
Life After Cancer: Kristy Elsberry
New program offers cancer survivors a helping hand.
Since her diagnosis, Kristy Elsberry has been fighting to beat cancer and keep it from coming back. That's why the 53-year-old wife, mother and grandmother joined Lake Regional's Re-Live program.
"There's no pill for me to take after chemo and radiation to help prevent the cancer from coming back," says Elsberry, who had triple-negative breast cancer. Other breast cancers can be treated for years with tamoxifen or Herceptin pills. "The only treatment I have left is to take out my risk factors, and diet and exercise will help me do that."
What Is Re-Live?
Re-Live is a new rehabilitation program at Lake Regional customized to the needs of patients who are receiving or who have completed cancer treatment.
According to the American Cancer Society, physically active cancer survivors have a lower risk of cancer recurrence and higher odds of cancer survival than those who are inactive. Exercise can also improve fatigue, cardiovascular fitness, muscle strength, anxiety, depression, self-esteem, happiness and other quality of life factors in cancer survivors.
"When we surveyed patients who had completed treatment at Lake Regional Cancer Center, they told us fatigue is their No. 1 challenge," says Lake Regional Cardiopulmonary Rehabilitation Director Jennifer Newman, R.N., CEN, cPT. "We developed the Re-Live program to help these survivors get their lives back."
Re-Live is an individual—not a group—program. Patients begin with an evaluation to determine their exercise regimen. Usually, the regimen includes a mix of using an exercise bike, arm bike (pedaled with the hands/arms), treadmill and weights.
"As their endurance improves, we increase the intensity and duration of their exercise, with the ultimate goal being 45 to 60 minutes of continuous exercise," Newman says.
Patients have medical oversight throughout the program, an important benefit for those who have completed treatment and who might go months before seeing a doctor.
"We are seeing those patients continuously and checking their vitals every time," Newman says. "That means we can see early signs of problems and help them connect with their doctors to get the care they need, whether that's a simple antibiotic or something major. This can help patients avoid hospitalizations."
More Than Physical Strength
At her first Re-Live appointment, Elsberry was surprised she couldn't complete her exercises.
"I thought, I've got to get back to good so I can garden this spring," she says. "Some people are writers, some are artists—everybody's got a God-given gift. Mine is in the garden."
Elsberry is a trained University of Missouri Extension Master Gardener. She creates beautiful landscaping at her home outside of Iberia, but last spring and summer, her treatments left her unable to use her gift. The sight of her neglected flower beds and vegetable garden saddened her, and she was determined to give them loving attention this spring.
She made progress her first couple of weeks at Re-Live, but then missed two weeks because of respiratory illness. She got in another week and then was sick again and missed two more weeks.
Such adversity is typical, Newman says.
"We expect patients who have undergone cancer treatment to have these setbacks, and we help them work through them," she says. "Also, evidence shows that being in a program like Re-Live can help patients come back from those illnesses sooner and stronger than they would otherwise."
Elsberry continued in the program and found it gave her more than physical strength. The continued care, she says, has also helped her manage cancer's mental and emotional tolls.
"I feel like I'm doing something for myself," Elsberry explains. "It might sound strange, but when my radiation ended, I felt like somebody had taken my umbrella on a rainy day. I thought, now what am I going to do? Well, I can do this. Modern medicine has done all it can for me, and now it's up to me to follow my doctor's advice."
Get Financial Help
Lake Regional Cancer Center patients with financial need may receive their first three months of Re-Live for free. To learn more about the financial assistance application, call Cancer Resource Navigator Nichole Stephens, LBSW, at 573.302.2752. Funding is provided by Lake Regional's Hope Program.
In the Fight: Robert Trokey
"Nobody can believe I've gone through this."
Robert Trokey was having a good time visiting with family at his brother's place on June 30, 2012, when suddenly, he felt faint and passed out. He quickly revived, but his niece, a registered nurse, still called an ambulance.
"I told her, 'No, I'm OK now,' but she insisted," says Trokey, who was 80 but in great shape. "I wasn't pleased at the time, but as it turned out, it was a good thing she did."
Once at Lake Regional, Trokey had a lung X-ray, which indicated a problem with his left lung. A CAT scan revealed a mass.
Because Trokey is a veteran—he served in the Military Police Corps between 1952 and 1956—he went to the Harry S. Truman Veterans' Hospital in Columbia for care. Further testing revealed he had small-cell lung cancer. He received chemo at Truman, but he came to Lake Regional Cancer Center for radiation therapy, which he needed every day, Monday through Friday, for six weeks.
"I couldn't have gone 120 miles to Columbia every day," explains Trokey, who amazed his care team by continuing to work as a night security guard at The Club at Old Kinderhook throughout his treatment. "Lake Regional was close, and that made things much easier."
Trokey's treatment lasted from Aug. 22, 2012, to Oct. 2, 2012. The treatments were successful, and for more than two years, Trokey was cancer-free. But in early 2015, a tumor appeared on his left lung. Testing revealed it was not a recurrence of his first cancer, but a different, non-small-cell lung cancer.
"For my second round of treatment, Lake Regional was able to work it out with the VA so that I could receive both my chemo and my radiation here," Trokey says.
In May 2015, Trokey became one of the first Lake Regional Cancer Center patients to receive radiation therapy with the center's new, state-of-the-art linear accelerator. The new equipment enables therapists to focus higher radiation doses on targeted cells, while minimizing doses to surrounding healthy tissue. Although this is the same kind of treatment—intensity modulated radiation therapy—delivered by the Cancer Center's previous linear accelerator, the new accelerator offers enhanced imaging and greater speed, both of which improve accuracy and further limit radiation to healthy tissue.
Receiving radiation, Trokey says, was easy and painless. He lay still on a table for about 12 minutes while the radiation was delivered. Later, he did develop some temporary blistering at the radiation site, a common side effect.
Throughout his care, Trokey found the Lake Regional care team to be exceptionally helpful and kind.
"I am so tickled I got to have them," he says. "They are very serious about their job, but there's also levity from time to time, and I like that. It's a heck of a lot more pleasant than working with stern people."
Less than a month after Trokey's final treatment, his Lake Regional radiation oncologist, Mark Bryer, M.D., said Trokey will receive regular checkups every few months to monitor for recurrence but at present, is considered without any evidence of disease.
Now 83, the cancer survivor is enjoying life. He takes care of his 25 acres near Climax Springs and frequently entertains friends and family.
"I feel good," Trokey says. "Nobody can believe I've gone through this. I'm very pleased with Lake Regional. They have treated me very well and are continuing to look out for me."
Beating Breast Cancer: Pattie Alkire
"When I would get down, [my care team] would lift me up."
Pattie Alkire tells her breast cancer survivor story with a smile. Yet, there were times during her battle when she struggled not to give in to sadness and fear.
"If you're going through cancer, there are going to be good days and bad days; you'll take one step forward and two steps back," she says. "There are times when you give up, but then you see other people fighting cancer and think, 'If they can do it, I can, too.'"
Pattie found her breast cancer while performing a routine self-exam in February 2014. She and her husband, Raymond, were enjoying life as empty nesters and spent much of their time hunting, fishing and camping on the Gasconade. They also liked to leave their phones at home, climb in their SUV and drive gravel roads, looking at wildlife and talking.
That life was suddenly threatened when Pattie felt a lump in her left breast. It was about the size of a pea, but just a week later when she had a mammogram at the Lake Regional Imaging Center, the lump had already grown to 3 centimeters in diameter. A biopsy done three days later at the Imaging Center revealed she had stage III breast cancer.
Pattie started chemo at Lake Regional Cancer Center within a week of diagnosis and later had a double mastectomy and radiation. She had the usual side effects from chemo, including nausea and loss of appetite. She lost 30 pounds and was exhausted. Still, she managed to continue working as an accountant at Central Ozarks Medical Center in Richland. Co-workers, friends and family encouraged her in her fight, and through it all, Raymond was by her side.
"I couldn't have asked for anyone better to go through cancer with," Pattie says. "He has been a core support for me."
Additional support came from her care team at Lake Regional Cancer Center.
"They were wonderful—the nurses, doctors, volunteers, everybody," Pattie says. "They treated me exceptionally well. They gave me warm blankets and pampered me and made me feel appreciated. Whenever I had questions, they didn't mind me calling and would help me get what I needed to feel better."
She adds that the compassion she received at Lake Regional Cancer Center made a "big difference" in her recovery. "Because if you know that someone cares if you get well or not, it makes you fight a lot harder," she says. "When I would get down, they would lift me up."
Pattie has been cancer-free since her double mastectomy in August 2014. She took her last Herceptin chemo treatment July 2, 2015, and has finished one of five years of taking a tamoxifen pill. She is feeling good and says surviving cancer has given her a whole new outlook on life.
"There are a lot of things that change after cancer," she says. "Things that used to upset you don't matter anymore, and little things you used to take for granted are important now. The most important thing to me right now is I can wake up, get out of bed, go to work and be me."
Cardiac Care
Return to the Finish Line: John Wolfe
An avid runner finds his footing after a serious heart scare
John and Jill Wolfe have made a lot of memories running together.
“Our whole family runs, our son and daughter and their spouses, too,” John says.
The family has entered several races, from 5Ks to half marathons. Lake Regional’s 2016 Fun Run/Walk is one run none of them will soon forget — because it came less than three months after John had triple bypass surgery.
“He could’ve run it,” Jill says of her husband . “He slowed down for us.”
Signs and Symptoms
John’s incredible recovery followed a terrible scare. In January 2016, the then-48-year-old was running four to six miles a day to train for the Bridge & Dam Half Marathon in Lake Ozark. He became concerned when he noticed he was getting slower and more out of breath.
“I thought I had the flu,” he says. “I felt achy and had bronchial symptoms and chest pains.”
He took a week off and then went to his treadmill. But his first workout triggered severe jaw pain, chest pain and a strange headache. Jill insisted he go the next day to see his doctor, Lake Regional’s James Neill, M.D.
John easily agreed. Despite being a runner and in great shape, he knew his heart could be in trouble. Several of his family members — including two siblings, a parent and two grandparents — had experienced a heart attack or needed heart surgery, or both, by the age of 40.
Aware of this history, Dr. Neill referred John on to Lake Regional Cardiologist Zubair Khan, who ordered an echocardiographic stress test to check John’s heart’s function. Irregular results prompted Dr. Khan to order an angiogram to get more information about the blood flow to John’s heart.
With the ordering of the second test, John expected to hear he had a minor blockage, or blockages, that would require one or more stents, a minimally invasive procedure. But the results revealed a more serious situation.
Three of John’s arteries into his heart had significant blockages. That meant he needed open heart surgery to create three new paths for blood to flow to his heart — or triple coronary artery bypass grafting.
Getting Up and Getting Out
The first emotion John felt when Dr. Khan delivered the diagnosis was anger at himself.
“Because I had been working hard the last 10 years not to be in that position,” he explains, adding he had started running to avoid heart problems. He also had been careful with his diet.
Dr. Khan understood John’s frustration and assured him all of his effort had not been for nothing.
“His heart disease is genetic, so no amount of exercise was going to prevent it,” Dr. Khan explains. “But, it was still good that he had exercised. For one thing, if he hadn’t exercised, he likely would’ve had problems earlier. Second, because he was in good shape, his surgery risks were lower. And third, he was in better shape for recovery.”
Soon enough, John realized Dr. Khan was right. He had surgery on a Sunday morning, spent three days in the ICU — “The whole ICU staff was amazing,” he says — and went home that Wednesday.
“One week after I was released, I was walking three miles,” he says. “That doesn’t mean it was easy. It would’ve been very easy to just sit in the recliner. But the more I did, the better I felt. Being a runner, I knew the hardest part is getting up and getting out the door.”
Heart Strong
The morning of the 2016 Lake Regional Fun/Run Walk, John and Jill were joined by their entire family — their son and his wife, their daughter and her husband, and their two grandsons — and to John’s surprise, everyone had matching shirts.
“I was really touched,” John says. “I’m blessed to have a family that would stick it out with me. They’ve been there every step.”
Now more than a year after his surgery, John is doing great, with no symptoms. This past summer, he even took a 10-day backpacking trip in Colorado with his son and a friend.
“I am just living my life without worrying about heart trouble slowing me down,” he says.
Join the Fun Run/Walk!
The 10th Annual Lake Regional Health System Fun Run/Walk, benefitting Cardiopulmonary Rehabilitation, is Saturday, May 6. Click here for details and to register.
Close to the Heart: Bob Bueltmann
Bassing Bob shares his heart story.
Bob Bueltmann was having lunch with his son Robbie and friend Marcus Sykora when the chest pain started.
"We were out on the deck, overlooking the lake, and talking about some fishing event coming up," says Bueltmann, an avid angler known around the lake as Bassing Bob.
The pain felt similar to esophageal spasms, which had previously bothered Bueltmann, so he took a nitroglycerin to ease the contractions. Five minutes later, he took another. Then another. And a few minutes later, still another. When 30 minutes passed and the pain had not eased, Sykora told Bueltmann he was taking him to Lake Regional Hospital.
"I knew we had good care right down the road, and I just don't take any chances," Sykora says.
Lake Regional Cardiologist Zubair Khan, M.D., FACC, says it was a good thing Bueltmann did not wait.
"He was having a small heart attack but was on his way to a big heart attack that could cause permanent damage to the heart muscle," Dr. Khan says. "It was imperative that he receive care."
'Phenomenal' Care
Bueltmann was already a patient of Dr. Khan's, having established care with him at Lake Regional Heart and Vascular in 2012. Bueltmann had moved to the lake from St. Louis after retiring at age 55 from a successful career in technology sales and business development.
Not ready for a full retirement, Bueltmann decided to combine his passions for entrepreneurship and bass fishing. He launched BassingBob.com, now a popular website for Lake of the Ozarks anglers.
Bueltmann quickly found a local cardiologist because he had a history of cardiac problems. Between 2009 and 2010, while still in St. Louis, he had multiple stents to improve blood flow in minor arteries. Six months after he began seeing Dr. Khan, he received another stent.
When Bueltmann arrived at the Emergency Department on Sept. 2, 2015, his chest pain was at a nine. An electrocardiogram, or EKG, taken within minutes of his arrival showed that although he was not having an acute heart attack, his heart was not receiving enough oxygen. The care he received in the ED was "phenomenal," Bueltmann says.
Just 37 minutes after arriving in the ED, Bueltmann was taken to the catheterization lab, where Dr. Khan discovered that Bueltmann's ramus artery—a branch of the left main coronary artery—was 99 percent blocked. Dr. Khan placed a stent to restore the artery's blood flow. He also saw that Bueltmann's right coronary artery was 90 percent blocked; he did not place that stent then but scheduled a second procedure for Sept. 22. Bueltmann was able to go home from the first stent about 24 hours after he had arrived in the ED. For the second stent, he spent one night at the hospital. Both procedures went well.
Personal Connections
Throughout his care, Bueltmann says, he took great comfort from the personal connections he felt with the Lake Regional care team.
"It was easy to build a rapport with people," he says. "I love that about this hospital. I grew up in St. Louis and had gone to much larger facilities. I would never say those doctors didn't care—it's just not the same feeling I have here. There's this community here."
Having witnessed Bueltmann's care, Sykora reports similar feelings.
"It was comforting to see the professionalism and care that we have right here, locally," he says. "It's so reassuring, and we're thankful to have Lake Regional here to help us."
Heart Set on Recovery: Carl Gauck
Heart attack patient Carl Gauck comes back strong with cardiac rehab.
 After
suffering a heart attack and undergoing heart surgery, Carl Gauck is
enthusiastically following his doctor's orders for cardiac
rehabilitation.
After
suffering a heart attack and undergoing heart surgery, Carl Gauck is
enthusiastically following his doctor's orders for cardiac
rehabilitation.
"My attitude is, anything that's going to help me get back to normal to do the things that I enjoy, I'm going to do it," says Gauck, a Lake Ozark resident who has served as the Missouri Senate chaplain for 18 years and who is completing his cardiac rehabilitation at Lake Regional Hospital.
Cardiac rehabilitation might look like regular exercise, but at Lake Regional, it's a personalized, three-part program aimed at healing and recovery.
"Cardiac rehabilitation is vital for individuals who have suffered a heart attack or stroke, or who have undergone heart surgery," says Jennifer Newman, R.N., CEN, cPT, Director of Cardiopulmonary Rehab at Lake Regional Health System. "Completing a program can reduce a patient's risk for future health problems, and patients in cardiac rehab also regain strength and confidence, which enables them to lead fuller, more active lives."
Me? A Heart Patient?
Gauck's heart attack came as a complete surprise. At age 73, he was getting 60 to 90 minutes of exercise five days a week and felt fit and strong. But on Aug. 24, 2015, he woke up with back pain. A couple of hours later, it moved to his neck and jaw. Although the pain was not severe, Gauck recognized it as a sign of a heart attack and went to Lake Regional Emergency Department, where Cardiologist Muthu Krishnan, M.D., FACC, confirmed his heart was not getting enough blood. Surgery to restore blood flow with a cardiac stent followed.
Dr. Krishnan prescribed cardiac rehabilitation three times a week for 12 weeks, the most common program schedule. In the first phase of the program, an educator visited Gauck while he was still hospitalized and discussed changes he needed to make to his medications, diet and exercise routine.
The second phase began after Gauck's discharge with an exercise consultation in the hospital's workout facilities. Staff evaluated his responses to various exercises by monitoring his blood pressure, heart rate and oxygen levels. The results determined which exercises he needed, as well as how intensely he should do them and for how long each time.
Completing the exercises was difficult at first, Gauck says.
"Although my heart function was fairly good, the medication I was on made me weak," he explains.
"Our house sits at the bottom of a hill, and he could hardly make it up the stairs," his wife, Janet, adds. "I'm surprised at how much strength he's gotten back."
Finding Support
At the end of his 12 weeks, Carl had improved but, as expected, still had farther to go. He enrolled in the cardiac rehab program's third phase, which gave him continued access to the workout facilities, as well as the nurses, dietitian and exercise physiologist who monitor his health status and regularly update his exercise prescription. The care team, Carl says, is "extremely knowledgeable and compassionate."
"They have a good sense of humor, too, which is important to me," he says. "It's not doom and gloom."
When Carl began the third phase, Janet took advantage of a program for spouses to also work out at the rehab facilities.
"I thought, 'It'll get me in shape,' and I did it to support and encourage him, too," she says.
More support has come from Carl's fellow patients.
"We've bonded over our similarities," Carl says. "There are three of us who started together and who come at the same time. That encouragement is important. I want to be here because of the relationships I've built."
The social aspect of cardiac rehab is important to most patients, Newman says.
"Cardiac rehab is about more than physical recovery," she says. "Patients also draw strength from the individuals working alongside them. Their shared experiences make friendship easy."
Moving Forward
Carl plans to continue his rehab at least until the one-year anniversary of his heart attack.
"The attitude of the staff—their encouragement—and the time with fellow patients make me want to be here," he says. "And, it makes me look forward to this spring and summer and being active again."
"Now, he goes up and down those stairs, no problem," Janet adds. "He's doing so good. I'm so proud of him."
Eleven Steps: Ron White
A simple climb revealed Ron White had a critical problem.
Ron White knew he was in trouble halfway into his climb up a flight of 22 stairs.
"I got to the eleventh step, and I had to stop," he recalls. "I couldn't breathe."
A couple of fishing buddies standing on the dock below ran to Ron's rescue. They convinced their long-time friend that a trip to the doctor was in order, even though Ron argued that he was in perfect health.
"I had a blood pressure of 120 over 70 for 40 years," Ron says. "That should count for something."
A visit to his primary care physician, James Neill, M.D., raised more red flags. Dr. Neill ordered an electrocardiogram (EKG), and his concern grew when he viewed the results.
"He wanted to do an electrocardiogram to find out if anything was wrong with my heart," Ron says. "That didn't come out so well."
Dr. Neill scheduled Ron for a cardiac catheterization, a procedure to determine how well the heart is working. Doctors insert a thin, hollow tube called a catheter into a large blood vessel that leads to the heart. Through the catheter, doctors can perform diagnostic tests and treatments on the heart.
In Ron's case, the tests revealed ominous news: He had critical blockages of the most important arteries in the heart. He needed immediate surgery.
The gravity of the situation weighed heavily on Ron and his wife, Debbie, as they went through the motions of preparing for Ron's surgery.
"I remember thinking at that point that our life as we know it is going to be very different," Debbie recalls. "We are going to have to find a new normal, and I was afraid that normal was going to be old."
Today, Debbie is happy to report that those early fears never came to fruition. Ron's Lake Regional care team was able to completely revascularize his heart, enabling him to resume a normal lifestyle with a life expectancy of many more years.
"They take a heart that's been repaired, and they make it into a heart that's normal,"Ron says. "As normal as it can be."
"Of course, he could not lift, couldn't do things at first," Debbie says. "But his doctor kept stressing that he was not an invalid. He needed to be up; he needed to be walking. We're where we are now because of that."
The next step was cardiac rehab, a task Ron enthusiastically embraced.
Cardiologists agree that cardiac rehabilitation is a critical component of the recovery process. Cardiac rehabilitation may look like regular exercise, but at Lake Regional, it's a three-part program with serious health benefits. Lake Regional's Cardiopulmonary Rehabilitation program is certified by the American Association of Cardiovascular and Pulmonary Rehabilitation.
"I'm working with a real super group at that hospital," Ron says. "They're a team; it's so obvious right from the start. From the prep rooms all the way through rehab, everything was professional."
Orthopedics
1 Surgery, 2 New Knees: Kristi McGrew
Local teacher has both knees replaced at Lake Regional
Kristi McGrew, a reading teacher at School of the Osage Heritage Elementary School, had an unusual summer project.
“While school was out, my summer project was to get new knees so I can keep up with all of the kids,” says McGrew, who has served School of the Osage for 20 years. “Anytime I was on my legs for an extended period, they would get so sore and achy.”
Early Signs of Knee Trouble
McGrew’s knee troubles began with a torn ACL when she was 25. She had surgery, but as often happens with ACL tears, the knee eventually developed osteoarthritis. As the cartilage in her knee wore away, McGrew experienced increasing pain and loss of movement.
Then last December, her left knee began to have similar problems. That’s when she began to wonder if a woman in her 50s could be a candidate for knee replacement surgery.
There are pros and cons to replacing joints in mid-life, says Jeff Jones, D.O., a board-certified orthopedic surgeon at Lake Regional Orthopedics.
“In the past, hip and knee replacements were performed only on patients ages 65 and older,” he says. “That’s because the new joint won’t last forever — in general, 20 years is a good expectation. But many people don’t want to wait until they are 65. Many decide, ‘I want good quality years now, and if needed, I’ll deal with a second surgery later.’”
That made sense to McGrew.
“For quality of life, I decided to go ahead,” she says.
2 Replacements, 1 Summer
Hoping to use up just one summer, McGrew was happy to learn she could have both knees replaced at once. And “at once” meant exactly that — Dr. Jones asked his fellow Lake Regional board-certified orthopedic surgeon Rick Walker, D.O., to operate alongside him, with each of them replacing a knee. The main benefit of this approach, Dr. Jones says, is a shorter anesthesia time.
“That’s a little safer for the patient,” Dr. Jones says.
To get ready for her surgery, McGrew attended Lake Regional’s Total Joint Camp. This two-hour class helps patients know what to expect before, during and after total hip or total knee replacement surgery. The camp includes tips from the orthopedic surgeons, as well as from physical and occupational therapists, dietitians and social workers.
“It took away a lot of the worry and fear because I knew what to expect,” McGrew says.
After surgery, McGrew spent four days at Lake Regional Hospital. The care, she says, was a perfect balance of professional and personal.
“Professional because everybody really knew how to do their job, and I felt safe,” she says. “And then also personal because I never felt like anybody was just doing their job. I felt like they really, genuinely cared about me. People were always asking, ‘Can I do anything for you?’ Not only the medical professionals — the techs, nurses, physicians — but also the housekeeping personnel and volunteers. I felt really thankful.”
After being discharged, McGrew decided to spend seven days at the Lake Regional Skilled Nursing Facility, located within the hospital. She received physical therapy twice a day and occupational therapy as needed.
“The best thing about the Skilled Nursing Facility was that I had an extra week to focus — just focus — on getting better and getting stronger,” she says.
At first, McGrew needed help to walk short distances. A couple of days later, she just let staff know when she’d be walking.
“Then the last couple of days, I could get up and walk around as I pleased because I was safe to do that,” she says.
Expert Care Close to Home
For the rest of her summer, McGrew went to the hospital three times a week for physical therapy. She switched to twice a week when school started.
“My physical therapists are wonderful about helping me with practical aspects of life,” she says. “They ask me what is challenging me and then show me exercises and other tips to help make these tasks easier and to help me get stronger and more flexible. There is some stiffness, but I have no pain in my joints. I am able to go up and down stairs and am getting faster when walking. I was still using a cane for the first week back to work but abandoned it the second week.
“I know a lot of people think they have to go to a bigger city to get good hospital care, like somehow, right here at home, it’s not going to be good enough,” she adds. “I didn’t experience that at all. My surgeons used the latest methods, and along with that professionalism, I had the personal aspect because I had nurses who were parents of kids I’ve had in school. I had people from the community I know, and that means a lot to me, to be in my community, where I know the people who are taking care of me.”
Field of Play: Denetria Lewin
A triple knee injury cannot keep Denetria Lewin down.
Fifteen minutes into a Friday night soccer game, high school athlete Denetria Lewin suffered a potentially career-ending injury.
"I went up for the ball with another girl, and our knees collided while we were in the air," Lewin recalls. "I heard a pop and felt instant pain."
In the world of competitive sports, that dreaded "pop" is an alarming sign of injury to the ACL—the ligament that helps stabilize the knee and prevents the shinbone from sliding out in front of the thighbone. Experts warn that ACL injuries are a growing problem for high school athletes, especially among females, who are three times more likely than their male counterparts to sustain such an injury.
ACL injuries have dashed the hopes of many an athlete. Without the proper treatment and physical rehabilitation, they can lead to joint instability that can significantly reduce an athlete's level of play and increase the risk of re-injury.
All this weighed heavy on Lewin's mind as she awaited the results of her MRI.
"I was definitely concerned that this could threaten my ability to get an athletic scholarship to help pay for college," Lewin says. "It wasn't a good situation."
Initially, the MRI results seemed to confirm her worst fear. Not only had Lewin torn her ACL, her MCL and meniscus were also damaged—a combination of factors that can wreak havoc on knee function and joint stability.
"It was very upsetting," Lewin says. "This is one of those career-type setbacks, and I had it."
In less severe cases, nonsurgical methods such as physical therapy, bracing and activity modifications are options for treatment. But when it comes to returning to the playing field, studies show that athletes who undergo ACL repair are more likely to return to activity at their previous level than those who opt out of surgical treatment.
After a consultation with Lake Regional Orthopedic Surgeon Scott Hofer, D.O., Lewin felt surgery was the best option. Several months of recovery and rehab later, she remains certain she made the right decision.
"I'm doing great, and I have no limitations," Lewin says. "I wear a sports brace for contact sports, but I still play soccer, and I play rec league volleyball, as well as running and ice skating."
Though he's pleased with Lewin's outcome, Dr. Hofer cautions that surgery is not a quick fix and stresses the importance of intensive therapy to the recovery process.
"Fortunately, she's done very well and feels that she's able to get back to the same level of play she had before, so she's definitely a success story," Dr. Hofer says. "But athletes should be aware that ACL repair doesn't guarantee a return to competitive sports.
"About 75 to 80 percent of patients will get back to competitive sports, but it will take about nine to 12 months to recover fully, and they'll need to make a serious commitment to physical therapy."
During the post-operative rehab process, physical therapists initially work with patients on restoring range of motion and getting the quadriceps muscles firing again so the injured leg can bear weight. From there, patients progress to more agility and sports-related activities.
Lake Regional Physical Therapist Holly Sabourin knows it can be challenging to work with athletes because they often want to exceed their capabilities, which can delay recovery time and sometimes lead to re-injury.
"Often athletes like Denetria want to do so much, and you're telling them they're not quite ready to do that yet," Sabourin says.
On the other hand, that same drive can be a great motivator when it comes to recovery. Sabourin credits Lewin's competitive spirit with playing a pivotal role in the athlete's impressive comeback.
"She did all of her homework assignments and worked really hard in all her physical therapy appointments," Sabourin says. "She was an easy, easy person to get better."
Now attending college in Arizona, Lewin commends the Lake Regional Sports Medicine and Rehab team for allowing her many more years of healthy competition.
"Dr. Hofer was great," Lewin says. "He was really helpful in giving us options and explaining things. Everyone was so helpful and caring. Overall, it was a great experience and a great outcome."
Mended Dreams: Jessi Whittle
High school athlete gets another shot after ankle surgery at Lake Regional.
From the look in her daughter's eyes, Kim Whittle knew something was wrong. After sliding into home, Jessi Whittle had not gotten up. Instead, the then-14-year-old looked for her mom, who was sitting behind home plate. Then, Jessi started to stand and Kim saw her daughter's right foot was turned sideways.
"I jumped up, called a timeout and ran onto the field," Kim says.
As Jessi collapsed back on the ground, she looked at her foot and immediately thought of basketball—her favorite sport. "I didn't think I'd ever get to play again, because of how my foot looked," she says.
Breaking News
An ambulance was called, and Kim requested transport to Lake Regional Emergency Department, where, she says, Jessi received "phenomenal care." Nurse Practitioner Tracy Sambolin immediately called Cody Fox, DPM, FACFAS, a Lake Regional sports medicine doctor who specializes in the foot, ankle and lower leg. X-rays revealed a broken ankle, and Dr. Fox ordered Jessi's ankle be stabilized and splinted and that she follow up with him.
Jessi and her mom later saw Dr. Fox in his office at Lake Regional Podiatry. He told them Jessi had a "classic ankle fracture pattern" and needed surgery. "We discussed what the risks, benefits, potential complications and expected outcome of the surgical intervention and injury would be," Dr. Fox says. "A classic ankle fracture pattern, when fixed, has a very good prognosis."
Saved by Surgery
Jessi had outpatient surgery at Lake Regional Hospital. Kim admits she was nervous before the procedure. "I asked Dr. Fox again what he was going to do, and he took the time to tell me," she says. "I can't say enough good about him and his staff that day."
The surgery restored the length of Jessi's fibula, stabilized her ankle and preserved normal ankle range of motion and function. "The challenge that I typically have with this type of injury is postoperative compliance with the non-weight-bearing protocol," Dr. Fox says. "Jessi is an athlete, and I wanted to ensure a speedy recovery without pushing too aggressively and returning her to sports activity too soon."
Shooting Star
Jessi followed Dr. Fox's orders and started physical therapy at Lake Regional, where she learned exercises that she's still doing to keep her ankle strong. "It felt long," she says of her recovery, "but it really wasn't that long." In fact, Jessi was back to sports in three months—in time for basketball season.
"Softball is just another sport she plays, but basketball is her life," Kim says. "To see her on the court was an amazing moment for a mom." Kim adds that if she had the choice again, she would want the same exact Lake Regional health professionals caring for her daughter.
"That's how great the care was," she says. "Here was this 14-year-old kid who thought her career was ending and Dr. Fox reassured her it wasn't—it was only going to get better."
A Hip Approach: Sue Parks
A new hip offers Sue Parks relief after osteoarthritis diagnosis.
 Sue
Parks was tired of limping, and she was tired of hurting. She had to do
something about her bad hip. "After work, I just went home, and that
was it," she says. "Once I made it to the recliner, I was done."
Sue
Parks was tired of limping, and she was tired of hurting. She had to do
something about her bad hip. "After work, I just went home, and that
was it," she says. "Once I made it to the recliner, I was done."
Finally, Parks went to see Jeff Jones, D.O., an orthopedic surgeon at Lake Regional Hospital. He diagnosed her with end-stage osteoarthritis in her right hip.
"In osteoarthritis, the cartilage that cushions the bones and serves as a shock absorber breaks down until, finally, there is no cushion left," he says. "The common description of this condition is bone-on-bone. It causes loss of movement and significant, often severe, pain."
The solution Dr. Jones recommended for Parks was hip replacement surgery. While the thought of surgery and recovery made her anxious, Parks agreed to the plan. "I wanted to get on with my everyday life," she says.
Faster Recovery with New Approach
Although living with a bad hip is never easy, Parks' job made it especially difficult. She works in materials management at Lake Regional, and part of her job is to deliver supplies using large two-tiered carts. It was painful getting around, but she kept going to work. "I was slower than everybody else, but I got it done," she says.
Before talking with Dr. Jones, Parks was concerned that having her hip replaced would require a long recovery. He explained that a procedure offered at Lake Regional would make recovery much easier than if she had a traditional hip replacement.
Known as the anterior approach, the procedure Dr. Jones and his fellow Lake Regional orthopedic surgeons perform does not require cutting any muscles or tendons. The surgeons use a Hana® table, a high-tech surgical table with moving parts that enable precise patient positioning. Surgeons are then able to access the hip joint from the front of the hip—instead of the back, which is the traditional way. The front, anterior approach allows surgeons to work through the natural gap between the muscles.
"Using the traditional, posterior approach, after we finished replacing the hip, we had to surgically repair the muscles and tendons we had cut," Dr. Jones says. "Because no cutting and repair is necessary with the anterior approach, patients recover much more quickly and with less pain."
The Hana® table also allows for X-ray imaging during the surgery, which improves outcomes. "This is a big improvement from the traditional approach, because we can see precisely what we're doing during surgery, instead of taking an X-ray after we're done," Dr. Jones says.
From her first appointment with Dr. Jones through her recovery, Parks was glad to be in his care. "He takes the time to explain things; that's what I like," she says. "I have a lot of respect for him."
Back to Work
Parks had her surgery in October 2014. Although she felt some soreness after the procedure, she immediately knew she'd made the right choice. "The pain I'd suffered with for more than a year, that was gone," she says.
The morning after her procedure, she could get out of bed, get out of a chair and even do something as simple as crossing her legs without fear of a dislocated hip. All of those actions would have been restricted with traditional surgery because of weak muscles.
Parks spent two weeks recuperating at Lake Regional, with the first week spent in a regular hospital room and the second in Lake Regional's Skilled Nursing Facility, located within the hospital.
After going home, she continued her therapy with three outpatient visits a week for five weeks. "I had Kevin Meglan the first two weeks of my physical therapy, and he was great with me," Parks says. "We were able to get a lot of exercises accomplished, including the stairs."
Parks returned to work in December and her co-workers were impressed with the difference in her. "I'm moving more quickly, and I've had people tell me I look happier," she says. "I have more energy, so now when I get home, I can go out with my dogs and cook dinner. I'm doing great. For anyone needing a hip replaced, I would highly recommend Dr. Jones and this surgery."
Thumbs Up for Exceptional Care: Tyler Delaney
Hyperbaric treatment helps 13-year-old keep his thumb.
At a reunion with Lake Regional Wound Healing Center staff members, 13-year-old Tyler Delaney was happy to give his former caregivers two thumbs up. After all, if not for the effort of orthopedic surgeon Scott Hofer, D.O., and the wound care team at Lake Regional, Tyler would likely be missing one of those thumbs today.
What was supposed to be a fun-filled vacation for Tyler's Wisconsin family nearly turned into a tragedy when Tyler's hand became entangled in a tow rope after a day of wakeboarding on the Lake of the Ozarks.
"As he was picking up the rope, the jet ski was still running," Tyler's father, Shawn Delaney, explains. "The rope got caught in the prop and got pulled in, which then wrapped around his thumb and dislocated it and almost pulled it off."
"When it immediately happened I thought I had lost my thumb," Tyler recalls. "As soon as I was told that I still had my thumb, I wasn't as worried, but I was still worried I could lose it."
Tyler's father rushed him to Lake Regional Hospital, where Emergency Department staff took immediate action to stabilize the wound and called in Dr. Hofer to determine if the thumb was salvageable.
"He sustained a circumferential laceration going around the finger with a fracture through the growth plate to the thumb," Hofer says. "He essentially nearly amputated the finger."
Initially, Dr. Hofer felt there was a 50-50 chance that Tyler might lose his finger. Half of the thumb had good circulation, but the nerve and blood vessel on the other half looked as though they were damaged beyond repair.
Fortunately for Tyler, youth was on his side.
"Kids heal a lot better than adults do," Dr. Hofer says. "Oftentimes, things that don't look salvageable are."
After cleansing and assessing the wound, Dr. Hofer realigned and stabilized the fracture by inserting a pin through the growth plate. He then repaired the skin lacerations with absorbable sutures.
With his thumb intact, Tyler was discharged into the care of his father. The pair hoped to salvage what was left of their time at the lake. But a follow-up visit to Dr. Hofer once again changed their vacation plans.
The tip of Tyler's thumb began to look dusky, and Dr. Hofer was worried the tip might die. He hoped the oxygen-rich environment of Lake Regional Wound Healing Center's hyperbaric chambers would improve oxygenation to the tissue and promote the healing process. Since opening in April 2009, the Wound Healing Center has used hyperbaric oxygen therapy to treat a variety of ailments, including diabetic wounds, bone and skin infections, and acute trauma arterial insufficiency.
"By increasing the oxygen in the atmosphere, we're improving the oxygenation of the tissues [even though there is not a good blood supply]," Dr. Hofer says.
Tyler ultimately spent the remainder of his vacation doing 10 two-hour stints in the clear, comfortable confines of a pressurized hyperbaric chamber—making him the youngest patient to receive hyperbaric treatment at Lake Regional. He passed the time watching movies and enjoying plenty of father-son bonding time with his dad sitting on the outside of the chamber.
"I had a different picture in my head from what the chamber was," Shawn says. "To see that...I could see him and he could see out was great."
After Tyler finished his treatments at Lake Regional, the family returned home to Wisconsin. However, Lake Regional made sure he would have the appropriate follow-up medical care. After an exhaustive search, Wound Healing Center Program Director Laurie Lowther was relieved to locate a center close to Tyler's home that had a pediatric surgeon on staff.
A year later, Tyler has full use of his thumb and is brushing up on his favorite musical pastime—drumming. For the Delaneys, it's a return to normalcy that would not have happened without the efforts of Lake Regional's doctors, nurses, technicians and support staff.
"They helped me out so much that we just had to come back and say thank you," Tyler says. "I'm sure we will be coming back for years to come."
Students, Sports & Safety: Lake Regional Athletic Trainers
Lake Regional athletic trainers help young athletes avoid injury.
From sprains to concussions, injuries are a part of school sports. To help students compete with fewer injuries—and to ensure proper care for injuries that do occur—athletic trainers from Lake Regional Sports Medicine attend practices and games at three local schools.Kaelin Hood, Zach Greco and Josh Lammertcover multiple sports at School of the Osage, Camdenton R-III and Morgan County R-II, at no cost to the schools.
"We are proud to support our local student athletes and to be there, increasing their safety as they compete in sports they love," Hood says. "Helping athletes be safe and healthy is not just a job but a passion for us."
A Win for Safety
The percentage of Missouri public schools with at least one full-time athletic trainer is on the rise, increasing from just fourpercent in 2010 to 2011 to 27 percent in 2014 to 2015, according to the Missouri State High School Activities Association.
"The national focus on athletes and concussion rates has put injury prevention at the forefront of sports medicine," says Scott Hofer, D.O., a board-certified orthopedic surgeon and sports medicine specialist at Lake Regional Orthopedics. "Parents, coaches and school administrators see the need to have proper prevention strategies in place."
Athletic trainers are health care professionals who specialize in nutrition; injury and illness prevention and assessment; and first aid and emergency care. Unlike personal trainers, who may or may not have higher education, athletic trainers must obtain, at a minimum, a bachelor's degree in athletic training, board certification and state licensure.
Brad Yoder, School of the Osage athletic director, says his district is grateful for the Lake Regional athletic trainers because their presence promotes student safety.
"Athletic trainers from Lake Regional provide us qualified and reliable attention for our athletes on a daily basis," Yoder says. "Furthermore, athletic trainers assist our coaches with assessing, maintaining and educating athletes for peak performance."
Yoder adds that not only are trainers crucial for dealing with immediate injuries, "but they are also important for rehabilitation that allows our athletes to quickly return to what they love—playing the game."
The Game Plan
Hood, Greco and Lammert use several strategies to minimize student injuries. To begin, they provide education to coaching staff and athletes on such topics as heat illness, proper bracing and concussion prevention. They also arrive at games and practices early and help the athletes take preventive measures, such as stretching and proper taping. Then, during the practice or game, the athletic trainers keep a close watch on the athletes, including those on the opposing team. If the trainers see or suspect an injury, they assess the athlete and, if necessary, start treatment.
“That first on-field assessment is crucial,” Lammert said. “This is where our skills can protect an athlete from causing further harm by continuing to play. My job is to get my athletes safely back on the field as fast as possible, and that process starts with treatment on the sideline on the day of the injury.”
If injured athletes require more care, Hood, Greco and Lammert can also see them at Lake Regional Orthopedics and Sports Medicine, where the athletic trainers assist orthopedic specialists with clinic patient care.
A Rewarding Career
The opportunity to be there for a patient from beginning to end is one reason the athletic trainers love their work.
"Seeing someone recover from an injury from start to finish and knowing that you were the one who helped them get through it is one of the most rewarding things about my career," Greco says.
Another draw is interacting with students.
"It's fun watching the kids I'm with every day play," Hood says. "You definitely get to know your athletes. I enjoy building those relationships."
Family Birth Center
Ireland's Arrival: Danielle and Aaron Ellsworth
Couple's nerves turn to joy with birth of first baby.
Wearing a bright pink headband and an ear-to-ear smile, Ireland Ellsworth flits from one person to the next during a reunion with the Lake Regional Family Birth Center staff. The 1-year-old seems eager to chime in as her parents share the story of her arrival.
"This was our first pregnancy, our very first baby, our first delivery," says Danielle Ellsworth. "I had no idea what to expect."
Nearly two weeks past her due date, Danielle was experiencing contractions but had no sign of dilation. As midnight became mid-morning, Danielle and her husband, Aaron Ellsworth, found comfort in knowing the doctors and nurses of the Family Birth Center were keeping a close eye on mother and baby with the help of fetal heart monitors.
"Fetal heart monitors are our eyes into the womb," says Lake Regional Family Birth Center Nurse Manager Mary Lou Gamm, RNC-OB. "We are in touch with what is going on with that labor every minute, regardless of whether we are standing right beside the mother's bed or watching the information on computers in the doctor's office or the nurse's station."
"It was very reassuring," Danielle says. "Hearing Ireland alive and well and her heart beating strongly was incredible."
As the hours crept by and Danielle still was not dilated, information from the fetal heart monitors became increasingly important. Danielle's obstetrician, Robert Nielsen, D.O., initially considered inducing labor, but the results of the monitoring indicated that it would put increased stress on baby Ireland.
"The nurses monitored her all night, and as my wife would have contractions, the baby's heart rate would drop," Aaron says.
Concerned, Dr. Nielsen decided the best course of action was to deliver by cesarean.
"Around 10 o'clock that morning, the doctor called for a cesarean section, and our daughter was born at 10:42," Aaron says. "It all happened very quickly."
More than a year later, the proud parents chuckle as Ireland toddles around the room in sparkly ballet slippers. They express gratitude for the Lake Regional care that helped them safely deliver their daughter.
"They were professional and dedicated to their job," Aaron says. "They took great care of my wife, and we have a beautiful daughter."
"It was a wonderful experience," Danielle agrees. "The nurses, Dr. Nielsen, all the staff—they were incredibly helpful. I can't say enough great things."
Breast-Feeding Success: Jessica Rozier
Jessica Rozier thanks Family Birth Center for a great experience.

In February, Lake Regional Family Birth Center earned designation as a Show Me 5 hospital. This recognition from the Missouri Department of Health and Senior Services goes to hospitals that adopt five evidence-based maternity care practices that support breastfeeding.
Jessica Rozier, a breastfeeding mom who had her first son, Brooks, in October 2012 and her second son, Liam, in September 2014, says her two deliveries at Lake Regional show the difference these practices make to moms and babies. With Brooks, Rozier had to explain to her care team that he should not be given pacifiers or formula. She also had to let them know that she wanted him in her room at all times.
Even then, he was taken out for his hearing test, and she worried he might get hungry and be given a pacifier.
But by the time Rozier had Liam, the Family Birth Center team was well on its way to being a Show Me 5 facility, and she could hardly believe the difference in support.
"Liam was placed on my chest immediately after birth, and he breastfed right away," she says. "I didn't even have to request that Liam be in my room—it was a given. I wasn't scared he'd be given a pacifier or that I would be told to supplement. He didn't even have to leave the room for the hearing test.
"This mama was very pleased to have a natural birth and a chance to really bond with my son in those crucial first few days," she continues. "I was wary about being able to have those moments in a hospital, but the staff at Lake Regional made them all possible."
The Show Me 5 Practices
- Help mothers initiate breastfeeding within the first hour of birth
- Practice "rooming-in," allowing infants to stay in the room with their mothers
- Give breastfeeding infants no other liquid, unless medically indicated
- Do not give pacifiers or artificial nipples to breastfeeding infants
- Foster the establishment of breastfeeding support groups and refer mothers to them on discharge
Big Care for Little Patients: Jennifer Hollingsworth
Lake Regional Family Birth Center nursery keeps family together.
When Jennifer Hollingsworth first heard that her 6-day-old daughter, Helen, needed to be readmitted to the Lake Regional Family Birth Center to gain weight, she felt a little panicked. Helen was expected to be fine, but to stay with her, Hollingsworth thought she'd have to be separated from Helen's twin brother, Quill. And she was breastfeeding both.
Thankfully, Hollingsworth didn't have to choose between her newborns.
"The doctors and nurses assured me that Quill could stay overnight, too," she says. "I was so relieved. It would have been very hard emotionally to be separated from either of my babies."
Expert Care, Close to Home
Keeping families like the Hollingsworths together was one reason Lake Regional Family Birth Center became a level 2nursery in 2014. This designation allows the Lake Regional team to provide care for infants with acute needs, including infants who require antibiotics, IV fluids, respiratory support, help with feeding and much more. As a result, babies are only transferred to another hospital if they require neonatal intensive care.
"Providing additional acute care services helps ensure babies born at Lake Regional get the healthiest start possible," says Josh Brickner, D.O., a pediatric and internal medicine hospitalist at Lake Regional. "Staying at Lake Regional also means they can begin bonding with their families right away."
For Hollingsworth, a kindergarten teacher at Camdenton's Dogwood Elementary School, and her husband, Ryan, being close to home was an important draw to Lake Regional.
"We wanted to go somewhere close, and we've heard nothing but good things about the Family Birth Center," Hollingsworth says.
The Hollingsworths had already used Lake Regional Family Birth Center for the arrival of the twins' older sister, Abaigail, in 2009. When they returned six years later, they were pleased to find several of the same nurses still there.
"The nurses have an excellent bedside manner," Hollingsworth says. "They explained everything to me I wanted explained. And you could tell they all really liked babies."
Terrific Support
During both pregnancies, Hollingsworth received care for high blood pressure, and with the twins, the condition forced her to go on bed rest at 28 weeks. Still, she managed to hold off their delivery until she was at 37 weeks and five days.
"I made it a really long time, and I know that's thanks to the care I received," she says.
She delivered the twins through a scheduled cesarean section on May 29, 2015. Quill weighed 6 pounds, 7 ounces, and Helen 5 pounds, 11 ounces.
The babies were in good health overall. Lake Regional Lactation Consultant Annie Havner, R.N., BSN, IBCLC, helped Hollingsworth and the twins get started with breastfeeding.
"The twins were losing weight before we left the hospital, so we were supplementing with formula," Hollingsworth says. "Annie showed me how to do syringe feeding and tube feeding [so a bottle was not introduced]. I was also given a hospital-grade breast pump to help encourage production. I was still able to bond and do skin-to-skin, which is important for breastfeeding and just establishing attachment in the beginning."
The babies were discharged on June 2 and came back the next day to check for jaundice and weight gain. That's when Helen's weight loss required her readmittance. She stayed one night.
"They made me feel very safe," Hollingsworth says about the Family Birth Center staff during Helen's stay. "I really wanted to breastfeed, and they did not force us to do the bottle right away. We tried other interventions first."
Although Helen did eventually need bottle supplementation from a high-calorie formula, the support Hollingsworth received enabled her to continue breastfeeding both Helen and Quill through Helen's short hospitalization and for several weeks after she returned home.
"The whole staff was positive and encouraging," Hollingsworth says. "Without that, I wouldn't have even tried to continue breastfeeding, and I'm so glad I did. The bond is almost magical. To know you're the one providing them with their nourishment—it's amazing."
Family Focus
Because Lake Regional offered level 2nursery services, Helen was close enough to home to make it easier for other family members, including Ryan and Abaigail, to continue bonding, too.
"I was allowed all the company I wanted and felt that staff was very accommodating," Hollingsworth says. "They were great with Abaigail and made her feel that her role as a big sister was very, very important. Abaigail also stayed until it was her bedtime."
Now, several months later, Helen and Quill are healthy and growing right on schedule.
"I am very happy that Lake Regional had a level 2nursery and was able to meet the needs of my family," Hollingsworth says. "I felt more comfortable knowing we would all be together."
Additional Services
Precious Progress: Mark McGrath
Born with health challenges, a young boy shines in pediatric therapy

“O-pen!”
Three-and-a-half-year-old Mark McGrath announces his plan before sliding his thumb and fingers into the scissors. He carefully opens the blades and inserts a pink straw between them.
“Close!” he says. He squeezes the scissors, and a piece of straw flies through the air. A moment later, another piece follows it.
“Great job!” cheers Mark’s occupational therapist, Lake Regional’s Danielle Baumgartner. Mark pauses to look at her and smile.
It’s easy to cheer for Mark. This playful, determined little boy has overcome many daunting challenges. Born with multiple abnormalities affecting his heart, brain, spine, palate and more, he has had so many surgeries that his dad and mom, Patrick and Marcela McGrath, have lost count. His many medical issues have led to various developmental delays, including in his speech and motor skills.
“His neurologist thinks by age 6 — with intensive therapy — he may be caught up,” Marcela says, noting Mark’s cognitive development is on target for his age. “He may not ever run the fastest, but he may be caught up and able to live an independent life.”
Helping Mark achieve his victories are his speech, occupational and physical therapists at Lake Regional Health System in Osage Beach. He sees his Lake Regional therapists twice a week, with back-to-back appointments. Being able to coordinate his care that way has been critical, Marcela says.
“Because this is long-term,” she explains. “He needs intensive therapy at least until age 5, maybe longer. For this to be sustainable, I need to have all three therapies in one place.”
When Mark began at Lake Regional just after his third birthday, he was only saying, “Mama” and “Papa.” Six months later, he was constantly surprising his parents with new words. “The other day, he looked up and said, ‘Plane!’ ” Marcela says.
Cutting with scissors is another new achievement. He also has gone from a slow walk with lots of falls to a fast walk with fewer falls, and he can jump now.
“I’ve been very impressed with the therapists, and it’s not just what they do here,” Marcela says. “I love that they’ve given me ideas on how I can work with him at home.”
More Locations for Pediatric Therapies
Lake Regional offers pediatric physical, occupational and speech therapies at three area locations: Eldon, Laurie and Osage Beach. For more info, visit our Pediatric Rehabilitation Therapies page.
Life After a Stroke: Joe Davinroy
Lake Regional helped Joe Davinroy recover his speech—and his golf game.
When Joe Davinroy retired after working more than 40 years as a pharmacist, he envisioned plenty of fishing, yardwork and a whole lot of golf. What he did not plan on was having a stroke.
"I retired in January 2014 and had a stroke just six months later," he says. "I'd never thought about having to learn to walk and talk again."
Davinroy's stroke hit early one morning in July. His wife, Carolyn, heard him moaning in his sleep around 3:30 a.m. and struggled to wake him. His speech was slurred, and the right side of his body was weak. She called 911.
The Road to Recovery
At the hospital, an MRI revealed Davinroy was having an ischemic stroke, which is caused from a blood vessel blockage. Lake Regional Neurologist Philip Kurle, M.D., ordered tPA, a clot-busting drug that, given in time, can restore blood flow and prevent further cognitive and physical problems.
When Davinroy woke up in the ICU, he felt thankful that he was awake and aware. However, he had suffered some significant effects, including reduced use of his right arm, impaired language and poor balance, which made walking difficult. His recovery included a week and a half at Rusk Rehabilitation Center in Columbia for intense, inpatient rehabilitation therapies, followed by several weeks at Lake Regional for outpatient physical, occupational and speech therapies.
"It was excellent, just excellent," Davinroy says of the care he received. "The people at Lake Regional are so accommodating and concerned about their patients. That impressed me so much, that feeling that they care. It's so important."
Back in the Swing of Things
It took Davinroy about six weeks to recover the use of his right arm and balance, but regaining his speech took double that time.
"[Lake Regional Speech Therapist] Laura Davis was a godsend," he says. "She pushed me and gave me the confidence to get back to normal interaction with folks. People tell me all the time that they'd never know I had a stroke."
And that includes people who see him back out on the golf course. He made his return last fall.
"The first time I got back out there, the first three balls I hit went about 20 yards to the right and into the woods," he says. "My wife asked, 'How were you before?' and I said, 'Well, about the same.'"
He laughs and adds: "So my stroke didn't improve my golf shot, but it's fun to get out there. That was a big deal for me. I'm thankful we have a hospital in this area that could give me the care I needed so I could get back to the retirement I had planned."
Candid about Colonoscopy: Barbara Morawitz
"I felt like: 'OK. It's going to be all right.'"
"I'm 65 years old, and you are supposed to have your first colonoscopy at 50," she says. "I kept putting it off."
She explains that even a trip to the dentist fills her with dread, so it took her primary care doctor, Lake Regional's James Neill, M.D., insisting she have the screening before she worked up the courage for the potentially lifesaving test. Still, she arrived at Lake Regional Outpatient Services so anxious she was "almost nauseous," she says.
Then, in the prep room, a kind, upbeat nurse entered. As soon as Jim McMahon, R.N., began caring for her, Morawitz says, she began to relax.
"He was just happy," she says. "I felt like: 'OK. It's going to be all right.'"
McMahon did such a good job of distracting her that Morawitz didn't even notice when he put in her IV.
Other nurses and techs who helped care for her also did a great job of putting her at ease, Morawitz says.
"I felt like I was their only patient that day," she says.
One way the team helped calm her nerves was through explaining what she should expect at each step.
"They were really good at communicating," Morawitz says. "That was true of the people in the operating room, too. The [certified registered] nurse anesthetist Kevin [Lockett] thoroughly explained everything."
Morawitz chose to have the procedure at Lake Regional because of her familiarity with the hospital. In the fall of 2012, she and her husband, who has since passed away, moved to the lake from Scottsdale, Arizona, after having a second home here for 10 years. She began volunteering once a week at Lake Regional Hospital last fall—to help others, meet people and just get out of the house. She was still a new volunteer when she had the colonoscopy done in early December and did not know her nurses or other care providers.
She volunteered in the outpatient waiting room and had seen several people check in for colonoscopies, which helped her gather her own courage.
"I thought, 'If they can do it, I can do it!'" she says.
Morawitz's sister, who lives in St. Louis, brought her to the appointment, and she, too, was impressed with Lake Regional's care.
"She commented she could not believe how nice all the nurses were," Morawitz says.
Morawitz's test results raised no concerns, and today, Morawitz chuckles as she tells how easy her first colonoscopy turned out to be.
"All of the nurses and caregivers acted like they enjoyed their work," she says, "and it made it almost fun."
Back in the Classroom: Katie Heinz
Teen misses little school after having tonsils, thyroid removed.
When Katie Heinz learned that she needed both a tonsillectomy and thyroid surgery, missing school was one of her first concerns.
"I love school," says the School of the Osage senior. "I love my teachers. I didn't want to miss."
Heinz's tonsils had bothered her since childhood. They were oversized, making it difficult for her to breathe. She had chronic sore throats and always sounded stuffed up. Plus, her obstructed airway caused her to snore—loudly.
"I stopped getting invited to sleepovers because I would snore so loud," she says.
Her thyroid problems began more recently. A few weeks into her senior year, Heinz noticed a lump on the front of her neck. Heidi Calipjo, M.D., at Lake Regional Clinic–Osage Beach, referred her to Edward Barns, M.D., FACS, at Lake Regional ENT & Audiology, with notes about the lump—a nodule on Heinz's thyroid—and Heinz's oversized tonsils.
One look at her tonsils and Dr. Barns understood why Heinz struggled.
"She had extremely large tonsils with obstructive symptoms and chronic cryptic tonsillitis," Dr. Barns says. "It was clear she would benefit from having them taken out."
It wasn't so clear what was wrong with her thyroid. Although not likely, cancer was a possibility. Because a biopsy might give inconclusive results, Heinz opted for a thyroid lobectomy, which would remove the nodule along with one of her thyroid's two lobes.
But first, she would get her tonsillectomy. Dr. Barns used thermal fusion, a state-of-the-art procedure that reduces pain and recovery time.
"The recovery period is typically half that of a traditional tonsillectomy," Dr. Barns says, explaining that by using direct heat and pressure to seal and divide soft tissue, thermal fusion reduces damage to surrounding tissues.
Heinz had the procedure on Oct. 14, 2015, and was back at school the very next day. It was hard, she says, but she was determined. Her throat was sore for about nine days. At her two-week appointment, she had no complaints.
Because she recovered so quickly, Heinz could have her thyroid surgery less than a month later. The nodule was about the size of a golf ball but was not cancerous. Heinz kept enough of her thyroid that it most likely will function normally. She returned to school the following Monday.
"I'm glad that I had Dr. Barns," she says. "He was great. I was a little scared, but he talked me through the whole thing. He's confident, which made me confident, and he cares."
Wounds Can Heal: Anna Franklin
Prompt treatment helps patient with venous insufficiency.
Anna Franklin, 84, knew she needed to see her doctor.
"I had what I call a water blister come up on my leg just above my ankle, and it burst," she says. "My doctor said I should go to Lake Regional Wound Healing Center to have it treated."
Tests showed Franklin's wound resulted from venous insufficiency, a condition in which veins in the legs do a poor job of sending blood back to the heart.
"Venous insufficiency causes increased pressure and swelling in the lower leg, and blisters can form as a result," says Lake Regional General Surgeon Justin Shatto, M.D., who cared for Franklin. "When her blister broke, it left an open ulcer."
The ulcer was 7.4 centimeters across, wider than a baseball, but it was only superficially deep—the right time to seek care, Dr. Shatto says.
"Prompt treatment prevents more tissue loss, making it easier to heal the wound," he says.
For Franklin, Dr. Shatto ordered medicated wound dressings, as well as compression bandages to relieve the effects of venous insufficiency.
"The people caring for me were always really nice and prompt," Franklin says. "Dr. Shatto was really good. He was helpful and kept me relaxed."
Franklin came to the Wound Healing Center once a week for seven weeks, never missing an appointment. At the end of the seven weeks, new skin covered the wound. Her leg had healed.
"Consistency is very important in wound treatment," Dr. Shatto says. "Ms. Franklin was a great patient, and therefore, she had a great outcome."
Excellent Care in an Emergency: Aadon Magruder
"She treated my son like he was her own"
 Nine-year-old
Aadon Magruder couldn’t wait to jump in the water. His family was
vacationing at his great-great uncle’s lake house, and Aadon loves
swimming. But as he started to jump, Aadon slipped on the dock and
collided with a metal ladder.
Nine-year-old
Aadon Magruder couldn’t wait to jump in the water. His family was
vacationing at his great-great uncle’s lake house, and Aadon loves
swimming. But as he started to jump, Aadon slipped on the dock and
collided with a metal ladder.
And just like that, Aadon had a major laceration on his right shin.
Aadon’s parents, Aaron and Kristin, rushed him to Lake Regional Emergency Department. Aadon’s 4-year-old brother, Kason, also came along.
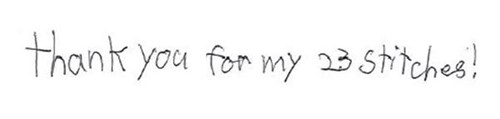
The care given to them all, Kristin says, was exceptional from the moment the receptionist greeted them until they were sent on their way — with 23 stitches on Aadon’s shin.
The first person to provide Aadon care was an ED triage nurse, Anne Wilson, R.N. She quickly packed and stabilized Aadon’s wound.
“Although most of the morning was a blur, I remember her thoughtfulness and kindness,” Kristin says.
Once in a treatment room, Kristin continues, Aadon was “enveloped with care” from nurses, radiology staff and “the angel in disguise” Nurse Practitioner Teresa Buol.
“When Teresa first entered the room, I knew Aadon was going to be OK,” Kristin says. “She treated my son like he was her own. She explained everything she was doing in ways that a 9-year-old would understand and made stitches sound cool. She repeatedly told him how brave he was and how proud she was of him. I was so impressed — just in awe. As a parent, watching my son go through something like this was horrible, but watching someone who actually cared and took time to make his leg look good and explain things to him to make him comfortable was worth the world to me.”
Kristin was so pleased with the care that she sent Lake Regional a note of thanks. She praised the various staff who helped them and ended the noted with: “You have a fantastic facility that I will recommend time and time again! This is the type of hospital that all hospitals should strive to be like. This is the kind of care that all patients should receive when they are ill. Thank you again for taking such good care of my son.”
And Aadon added a special PS:
Living Well with Lymphedema: Deborah Roehl
Occupational therapy helps relieve painful swelling

Deborah Roehl and Danielle Baumgartner, an occupational therapist at Lake Regional
Deborah Roehl had been free from uterine cancer for about a year when she noticed her ankle swelling. Her doctor prescribed Lasix and antibiotics, but the swelling and pain worsened — and then spread.
“In a little more than a year, I put on more than 100 pounds, and my leg was huge,” Roehl says.
Incurable but Treatable
Roehl had lymphedema. This condition occurs when the body’s lymphatic system has trouble circulating lymph, a clear fluid that surrounds cells and contains cell wastes. The poor circulation causes lymph to back up, resulting in severe, painful swelling.
Various diseases and conditions cause lymphedema, including congestive heart failure, chronic venous insufficiency and cancer. For Roehl, the trigger was radiation given to treat her uterine cancer.
Lymphedema cannot be cured, but it can be managed. Lymphedema therapy is one treatment that can help. Lake Regional occupational therapists provide this therapy, which uses a variety of techniques to improve lymph circulation. Manual lymph drainage uses gentle massage to draw fluid out of the tissues and back into the lymphatic system. Compression bandaging wraps the affected limbs to support circulation. And pneumatic pumps use inflatable “sleeves” to stimulate the flow of fluid.
“I’ve seen patients improve dramatically, from barely walking to living active lives,” says Lake Regional Occupational Therapist Katie Kelley.
Determined to Get Better
Before her cancer, Roehl was an active wife and mother who ran a daycare out of her home. After beating cancer, she was active again — until lymphedema. For more than 10 years, she struggled to manage the condition, but the swelling forced her to use a wheelchair. She continued to gain weight, and she had several bouts of cellulitis, a serious skin infection. In early 2015, the infection sent her to the hospital. Doctors weren’t sure she’d live.
“Hope is a powerful thing, and I had gotten to the point where I had lost my hope,” Roehl says.
Yet, knowing her life was in danger did something for Roehl. It took three weeks, but she left the hospital, determined to do whatever it took to get better. Roehl had been receiving therapy at Lake Regional Clinic – Eldon for a few years, but after her hospitalization, she came with a new attitude.
“She was different,” says Kelley, who had worked with Roehl since 2013. “She made a decision, ‘I’m going to do this this time.’”
That determination has brought results. Since July 2015, Roehl has lost 95 pounds and seen her whole life change.
“This last year has been awesome,” she says. “I’m more energized, more active. I’m walking all over the place. No more wheelchairs, no more hospital bed, no more blood pressure meds, no more diabetic meds. I’m doing things I’ve only dreamed of doing for 10 to 15 years. I can take care of my own house, fix my own meals — do everything myself. I’m excited to be alive again.”
Get Support!
Looking for lymphedema support? Check out these Lake Regional offerings:
Lymphedema: You Are Not Alone! This free support group, led by Lake Regional occupational therapists, meets at 5:30 p.m. on the third Wednesday of each month at Lake Regional Clinic - Eldon. Call 573.302.2230 for information.
Lymphedema 101. This free class at Lake Regional Cancer Center educates individuals who have lymphedema, as well as those at risk for developing the condition. Visit www.lakeregional.com/events or call 573.302.2772 for information.